Targeting KRAS in cancer has been a 40-year quest by scientists and researchers around the world. As director of inflammation and oncology research at Amgen, Rusty Lipford has devoted his career to developing therapeutics for a variety of cancers, and his team is instrumental in investigating KRASG12C at Amgen. Lipford recently recorded a conversation with Aaron Horowitz, co-founder and CEO of Sproutel, published on Amgen’s KRAS Information Center, where he describes how scientists first discovered the KRAS oncogene, and how lessons learned over decades of failures led to this innovation.
The following has been adapted from that conversation.
What is KRAS and how is it connected to some cancers?
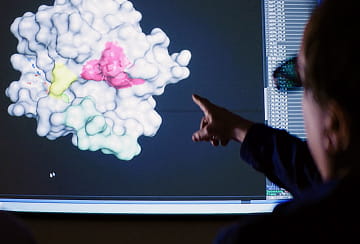
KRAS is an oncogene, which is a gene known to drive the growth of tumors if it mutates. Scientists have found KRAS to be mutated in a number of human cancers, including around 13% of patients with NSCLC. The KRAS gene was initially discovered about 50 years ago by scientists who were studying viruses that caused cells in a tissue culture plate to grow uncontrollably.
“KRAS was one of the original genes that they found that allow viruses to promote the uncontrolled growth of those cells,” Lipford says. “Then about 10 years later, they discovered that this KRAS gene in the virus actually corresponded to a human gene, marking one of the original discoveries of an oncogene.”
Flipping a “master switch” in tumor cells
All cancers are driven by genes and proteins that go rogue, causing uncontrolled cell growth. Scientists know that KRAS is one of the “master switches” that control cell division in human cells. But if it mutates, that switch can be permanently activated in the “on” position, leading to the uncontrolled growth of tumor cells.
In science, failures can guide the way
The search for ways to inhibit the tumor growth caused by KRAS mutations has been 40 years in the making.
“Science is built upon basically 90% failures, which tell you which direction not to go,” Lipford says. “We have 40 years of failure behind us — all of these years of people doing fantastic work to figure out just how nefarious KRAS is. That’s the way science works, and it makes the success all the more compelling and convincing.”
Testing for KRAS mutations is another piece of the puzzle
Proactive biomarker testing is a key part of any treatment plan. Testing for emerging biomarkers can often be accomplished as a part of larger biomarker testing panels. Many expanded testing panels already include KRAS, and KRAS testing in NSCLC is currently recommended by guidelines and professional societies.1,2,3

Ultimately, broader identification of mutations that drive cancer growth have the potential to lead to advances in patient care. Knowledge is the healthcare provider’s ultimate weapon in cancer therapy, informing a personalized treatment plan that’s best for each patient.
References
- Lindeman NI, Cagle PT, Aisner DL, et al. Updated molecular testing guideline for the selection of lung cancer patients for treatment with targeted tyrosine kinase inhibitors: guideline from the College of American Pathologists, the International Association for the Study of Lung Cancer, and the Association for Molecular Pathology. J Thorac Oncol. 2018;13:323-358.
- Kalemkerian GP, Narula N, Kennedy EB, et al. Molecular testing guidelines for the selection of patients with lung cancer for treatment with targeted tyrosine kinase inhibitors: American Society of Clinical Oncology Endorsement of the College of American Pathologists/International Association for the Study of Lung Cancer/Association for Molecular Pathology Clinical Practice Guideline Update. J Clin Oncol. 2018:36;911-919.
- Leighl NB, Page RD, Raymond VM, et al. Clinical utility of comprehensive cell-free DNA analysis to identify genomic biomarkers in patients with newly diagnosed metastatic non–small cell lung cancer. Clin Cancer Res. 2019;25:4691-4700.