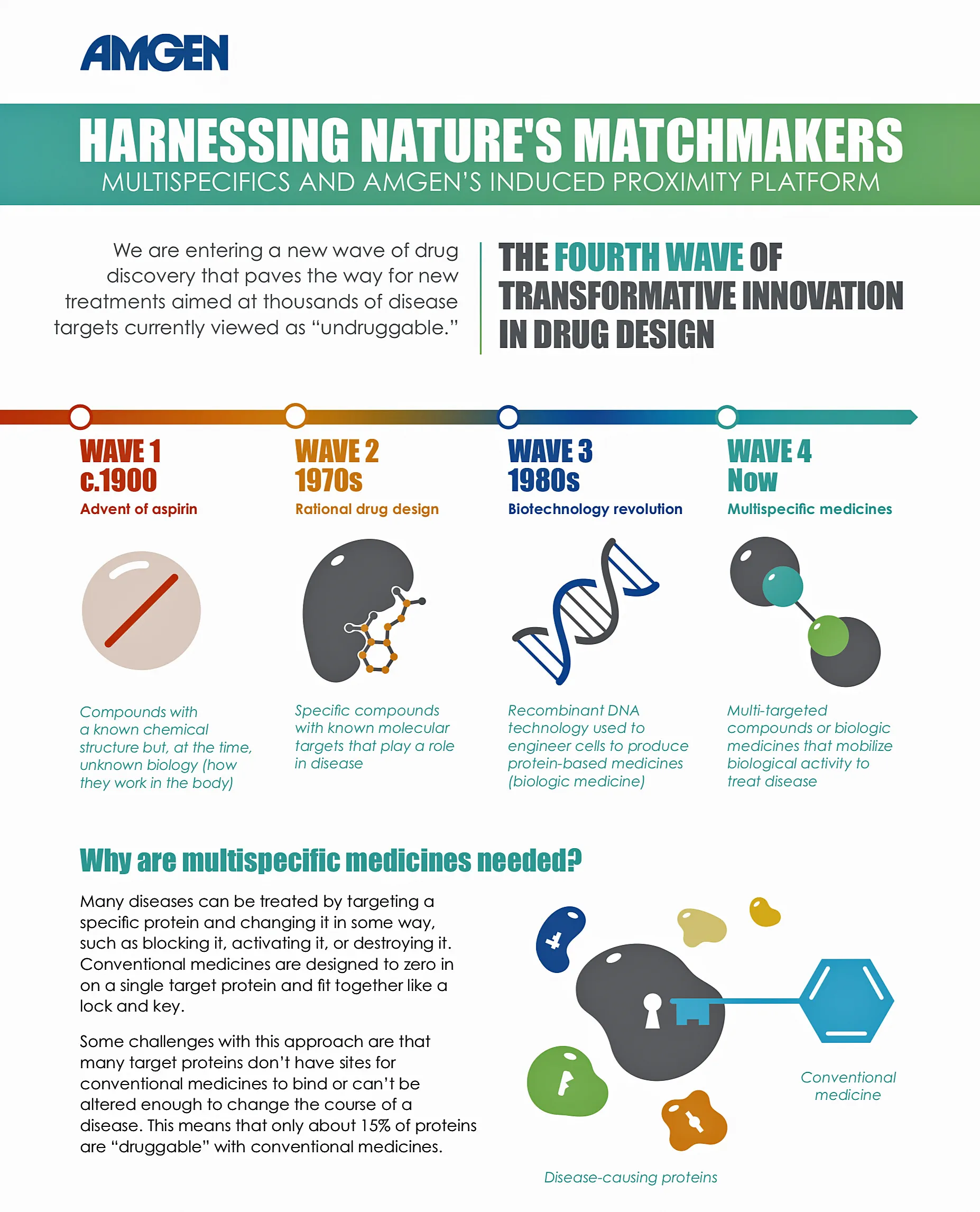
Why can heart attacks or strokes happen to people who appear to be perfectly healthy? There's a specific type of LDL called Liproprotein(a) that is emerging as an important potential risk factor for cardiovascular disease.1 Unfortunately, it's rarely considered until its impact is felt. Here are 8 things to know about this quiet threat.
1. Lp(a) is underappreciated.
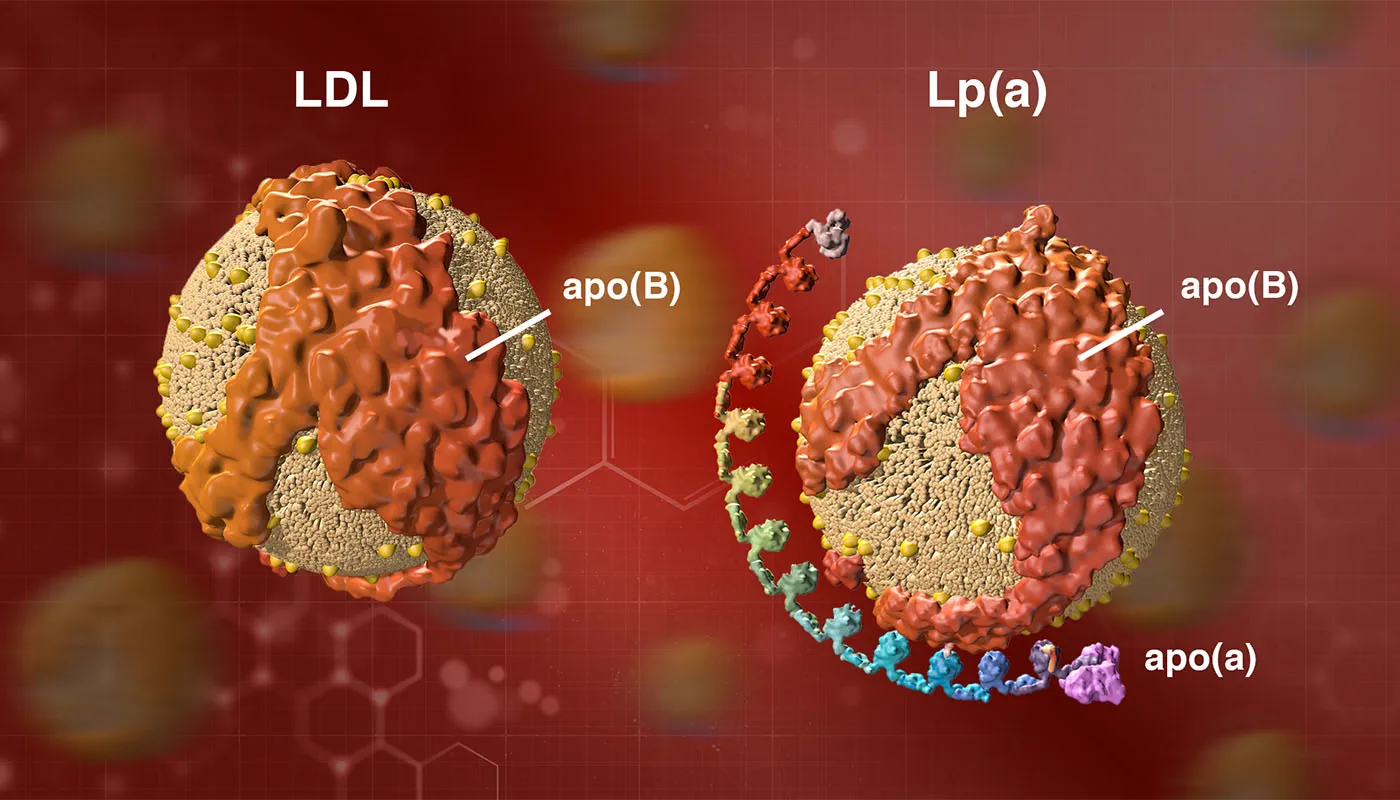
While most people know that low-density lipoprotein (LDL)-C, or "bad" cholesterol, can cause heart disease, relatively few people know about the potential risk posed by lipoprotein(a), or Lp(a).2 Yet it's estimated that up to 20% of people worldwide have high levels of Lp(a),3 which is associated with a person's risk of experiencing a heart attack or other serious cardiac event.1 Also referred to as "LP little a," this type of lipoprotein is comprised of an extra protein, called apolipoprotein(a) or apo(a),4 that is stickier than other types of LDL, so it may be more likely to cause blockages and blood clots in your arteries.5 As a result, high levels of Lp(a) may mean you are at a higher risk for heart disease, stroke, and other serious conditions related to blockages in your arteries.5
Despite the association between Lp(a) and heart attack, it flies under the radar of many physicians and remains infrequently measured in routine clinical practices.6 Even cardiologists may overlook Lp(a),7 in part because it is not as well-understood as other risk factors and treatment options are still very limited (see below).6
2. Lp(a) is a presumed independent risk factor for heart disease.

Previously, many cardiologists believed Lp(a) was only a concern for patients with other cardiovascular disease (CVD) risk factors, such as high LDL cholesterol. Research has suggested that Lp(a) is an independent risk factor linked to heart disease, even in younger adults and otherwise healthy people with no other known CV risks.1 Emmy-Award-nominated actress Marin Hinkle has a family history of elevated levels of Lp(a) contributing to heart disease.8 Sandra Tremulis, founder of the Lipoprotein(a) Foundation, was diagnosed with a 95% blockage in one of her coronary arteries at age 39.9
3. It's genetic.
Having an elevated Lp(a) is almost entirely determined by the genes you inherit, specifically the LPA gene.10 In fact, Lp(a) levels are 70% to 90% genetically determined.11 Unfortunately, lifestyle changes such as diet and exercise do not reduce Lp(a), and most of the commonly used preventive strategies for those with risk factors for CVD are ineffective. But people with high levels should still practice healthy habits, in consultation with their doctors, to reduce their overall risk of heart disease.12
As a result of this strong genetic influence, race-based disparities in Lp(a) concentrations have been documented, with Black individuals more likely to have elevated Lp(a) than Whites, Hispanic, or Asian individuals.13 Numerous case-control and prospective studies have consistently shown that Black individuals have two- to three-fold higher Lp(a) levels than Whites.13 More research and improved testing methods are needed to better understand the influence of race and ethnicity on Lp(a), and quantify the risks of elevated Lp(a) in different types of patients.13
4. People with lower overall LDL-C may have high Lp(a).

Since the cholesterol component of Lp(a) is incorporated in the LDL cholesterol laboratory measurement, your Lp(a) level contributes to your overall level of LDL-C that is measured by blood tests.5 The cholesterol portion of Lp(a) is referred to as Lp(a)-C.14 If your Lp(a) level is low, its impact on total LDL-C can be minimal. But in patients with high or very high Lp(a), their Lp(a)-C can account for much or most of their LDL-C test results.
For example, two people with similar LDL-C levels of 100 mg/dL could have very different heart disease risks. One person could have an Lp(a) level of 10 mg/dL, meaning that only about 10% of their LDL-C is derived from Lp(a)-C. The other person could have an Lp(a) level of 150 mg/dL, meaning that half of their measured LDL-C is actually Lp(a)-C. That's why testing for Lp(a) is so important, especially in people who have recurrent cardiovascular events despite LDL-lowering therapy.
5. Know your Lp(a) number.

Knowing your Lp(a) level can give you a better understanding of your risk for heart disease, stroke, and other blood vessel diseases than a routine cholesterol test that only measures your total LDL cholesterol level.15 If a large percentage of your LDL cholesterol is carried by Lp(a) particles, your risk for heart disease and stroke could be higher than predicted by routine cholesterol tests.5
Lp(a) testing should be considered in patients who are at high risk for CVD including people with:
- Premature heart disease or a family history of premature heart disease.16
- A familial history of high Lp(a).16
- Familial hypercholesterolemia (FH).16
- Recurrent cardiovascular events despite optimal LDL-lowering.16
- A 5% or greater risk for a fatal CV event within 10 years.16
6. Accurate and standardized tests are needed
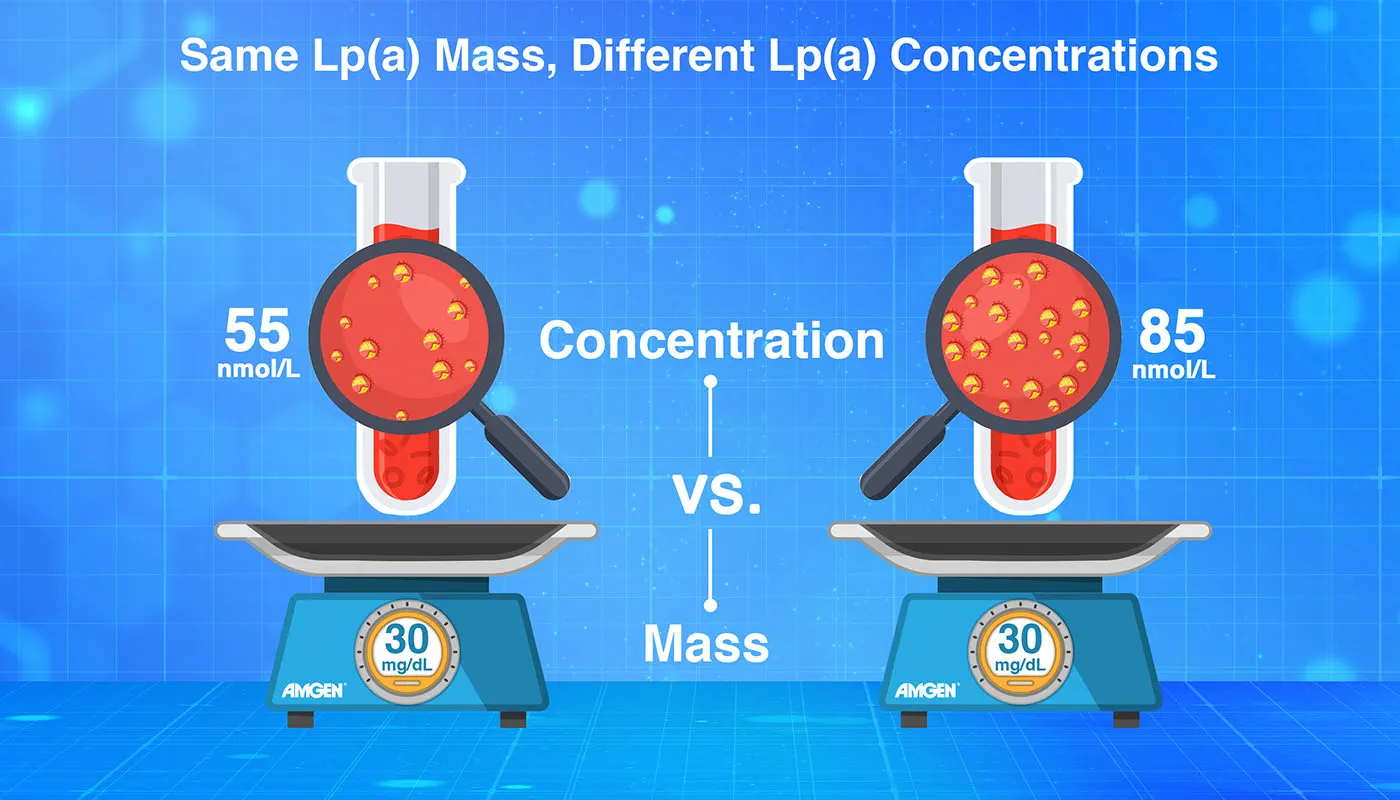
Because Lp(a) particles vary in size, the most commonly used lab tests are not ideal.17 These tests measure the total mass of Lp(a) in the blood in milligrams per deciliter (mg/dL).17 A more accurate approach is to measure Lp(a) in nanomoles per liter (nmol/L), which tells you the number of particles in your blood, not just the mass.17
Physicians and researchers specializing in this blood lipid have called for the development of more accurate, standardized tests that measure Lp(a) in nanomoles per liter. More precise testing methods will help physicians to better identify high-risk patients and support research into the potential link between Lp(a) and heart disease.
7. There are no approved treatments – For now!

Lp(a) has remained an elusive target since it was first discovered almost 60 years;18 common lipid lowering therapies have largely proven ineffective.19 Statins, the most widely used type of LDL-lowering drugs, do not reduce Lp(a) and may even cause a slight increase.20 Niacin (vitamin B3) can provide modest reductions in Lp(a), but it is not approved for the treatment of Lp(a).21 Moreover, large studies have failed to show that niacin reduces heart disease risk, and it may cause serious side effects in some patients.22
Any medicine designed to lower Lp(a) levels will require large cardiovascular outcomes studies to show that it can actually reduce the risk for heart attacks, strokes, and other serious events. According to one study based on genetic data, a large reduction in Lp(a) may be needed to achieve a meaningful reduction in risk.23
Luckily, thanks to new research in this area, there are treatments on the horizon that could potentially help those with elevated Lp(a) levels.24
8. Amgen is working on a medicine to silence the LPA gene.
In collaboration with Arrowhead Pharmaceuticals, Amgen is exploring a new type of therapy called short interfering RNA (siRNA) to treat high Lp(a). This approach targets and disrupts the messenger RNA that is required to translate the LPA gene into particles of Lp(a).25 By silencing the gene, the goal is to achieve a large and durable reduction of Lp(a).
References:
- Centers for Disease Control and Prevention. (2022, June 27). Lipoprotein (a). Retrieved October 28, 2022, from https://www.cdc.gov/genomics/disease/lipoprotein_a.htm
- HDL (good), LDL (bad) cholesterol and triglycerides. www.heart.org. (2022, June 20). Retrieved November 2, 2022, from https://www.heart.org/en/health-topics/cholesterol/hdl-good-ldl-bad-cholesterol-and-triglycerides.
- Wilson, D. P., et al. (2022). Use of Lipoprotein(a) in clinical practice: A biomarker whose time has come. A scientific statement from the National Lipid Association. Journal of clinical lipidology, S1933-2874(22)00244-6. Advance online publication. https://doi.org/10.1016/j.jacl.2022.08.007.
- MD, M. M. G. (2020, December 8). Lipoprotein (a): Five things you should know. Family Heart Foundation. Retrieved October 28, 2022, from https://familyheart.org/lipoprotein-a-5-things.
- U.S. National Library of Medicine. (n.d.). Lipoprotein (a) blood test: Medlineplus medical test. MedlinePlus. Retrieved October 28, 2022, from https://medlineplus.gov/lab-tests/lipoprotein-a-blood-test/.
- Khan, T. Z., Bornstein, S. R., & Barbir, M. (2019). Lipoprotein(a): the underutilized risk factor for cardiovascular disease. Global cardiology science & practice, 2019(2), e201911. https://doi.org/10.21542/gcsp.2019.11.
- Shapiro et al. 2019, Lipoprotein(a) Removal Still a Mystery. https://doi.org/10.1161/JAHA.118.011903Journal of the American Heart Association. 2019;8.
- Brooks, A. (2020, February 19). 6 celebrities connected to heart disease. EverydayHealth.com. Retrieved October 28, 2022, from https://www.everydayhealth.com/heart-health/celebrities-walking-the-aha-fashion-show/.
- The Lipoprotein Foundation. (2013, November 16). HIDDEN HEART RISK REVEALED: NEW NON-PROFIT EMPOWERS ~ 30% OF AMERICANS AT RISK FOR CARDIOVASCULAR DISEASE TO BE ADVOCATES FOR THEIR HEART HEALTH [Press Release]. Retrieved November 4, 2022, from https://news.cision.com/tremulis/r/hidden-heart-risk-revealed--new-non-profit-empowers---30--of-americans-at-risk-for-cardiovascular-di,c9499377.
- AHA names top heart disease and stroke research advances of 2020. www.heart.org. (2021, December 16). Retrieved November 4, 2022, from https://www.heart.org/en/around-the-aha/aha-names-top-heart-disease-and-stroke-research-advances-of-2020.
- Reyes-Soffer, G., et al. (2022). Lipoprotein(a): A Genetically Determined, Causal, and Prevalent Risk Factor for Atherosclerotic Cardiovascular Disease: A Scientific Statement From the American Heart Association. Arteriosclerosis, thrombosis, and vascular biology, 42(1), e48–e60. https://doi.org/10.1161/ATV.0000000000000147.
- Mackinnon, L. T., et al. (1997). Effects of physical activity and diet on lipoprotein(a). Medicine and science in sports and exercise, 29(11), 1429–1436. https://doi.org/10.1097/00005768-199711000-00007.
- Guan, W., et al. (2015). Race is a key variable in assigning lipoprotein(a) cutoff values for coronary heart disease risk assessment. Arteriosclerosis, Thrombosis, and Vascular Biology, 35(4), 996–1001. https://doi.org/10.1161/atvbaha.114.304785.
- Yeang, C., et al. (2021). Novel method for quantification of lipoprotein(a)-cholesterol: implications for improving accuracy of LDL-C measurements. Journal of lipid research, 62, 100053. https://doi.org/10.1016/j.jlr.2021.100053.
- Centers for Disease Control and Prevention. (2022, October 24). Get a cholesterol test. Retrieved October 28, 2022, from https://www.cdc.gov/cholesterol/cholesterol_screening.htm#:~:text=The%20cholesterol%20test%20checks%20your,)%20or%20%E2%80%9Cgood%E2%80%9D%20cholesterol.
- Lipoprotein(a) in clinical practice. American College of Cardiology. (n.d.). Retrieved November 4, 2022, from https://www.acc.org/latest-in-cardiology/articles/2019/07/02/08/05/lipoproteina-in-clinical-practice Cegla, J., et al. (2021). Lp(a): When and how to measure it. Annals of clinical biochemistry, 58(1), 16–21. https://doi.org/10.1177/0004563220968473.
- Cegla, J., et al. (2021). Lp(a): When and how to measure it. Annals of clinical biochemistry, 58(1), 16–21. https://doi.org/10.1177/0004563220968473.
- Koschinsky, M. L., et al. (2022). The long journey of lipoprotein(a) from cardiovascular curiosity to therapeutic target. Atherosclerosis, 349, 1–6. https://doi.org/10.1016/j.atherosclerosis.2022.04.017.
- Handhle, A., et al. (2021). Elevated Lipoprotein(a): Background, Current Insights and Future Potential Therapies. Vascular health and risk management, 17, 527–542. https://doi.org/10.2147/VHRM.S266244.
- Tsimikas S. (2016). Lipoprotein(a): novel target and emergence of novel therapies to lower cardiovascular disease risk. Current opinion in endocrinology, diabetes, and obesity, 23(2), 157–164. https://doi.org/10.1097/MED.0000000000000237.
- Lipoprotein(a) in clinical practice. American College of Cardiology. (2019, July 2). Retrieved October 28, 2022, from https://www.acc.org/latest-in-cardiology/articles/2019/07/02/08/05/lipoproteina-in-clinical-practice.
- Schandelmaier, S., et al. (2017). Niacin for primary and secondary prevention of cardiovascular events. The Cochrane database of systematic reviews, 6(6), CD009744. https://doi.org/10.1002/14651858.CD009744.pub2.
- Lamina, C., et al. (2019). Estimation of the Required Lipoprotein(a)-Lowering Therapeutic Effect Size for Reduction in Coronary Heart Disease Outcomes: A Mendelian Randomization Analysis. JAMA cardiology, 4(6), 575–579. https://doi.org/10.1001/jamacardio.2019.1041.
- O'Donoghue, Michelle (2022, November 5-7). Reduction of Lipoprotein(a) With Small Interfering RNA: The Results of the Ocean(a)-DOSE Trial (OCEAN(a) DOSE) [Conference Presentation]. American Heart Association Scientific Sessions, Chicago, Illinois.
- Swerdlow, D. I., et al. (2021). Treatment and prevention of lipoprotein(a)-mediated cardiovascular disease: The emerging potential of RNA interference therapeutics. Cardiovascular Research, 118(5), 1218–1231. https://doi.org/10.1093/cvr/cvab100.